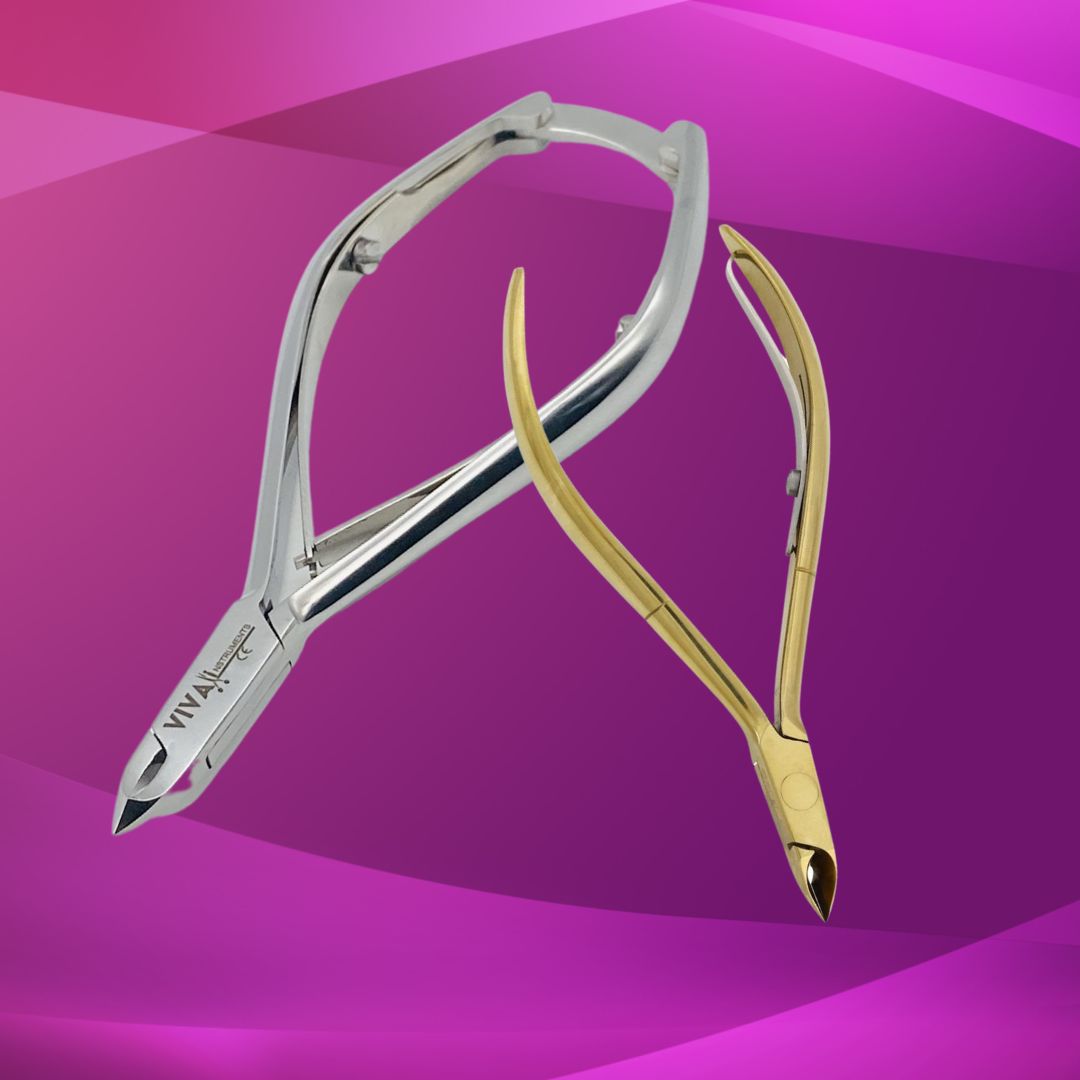
Beauty & Surgical instruments are designed to perform many specific functions. The use of any instrument for tasks other than those for which they are intended may result in damage or breakage. The proper cleaning, handling and sterilization procedures will ensure that your surgical instrument will perform as intended and extend its useful life.
How Supplied
The instruments are supplied non sterile and must be cleaned and sterilized prior to use according to the procedures outlined in this document, unless stated otherwise with the packaging of the product.
Inspection & Function Testing
Visually inspect and check the instruments for damage and wear and that the slots and any threads on collected handles are undamaged.
Precautions
Use caution during cleaning and sterilization as the handles require special handling to prevent damage. To avoid damage to the handle's bayonet fitting end and threads on collected handles during cleaning or sterilization, a tumbling action should be avoided. Instruments manufactured from different metals (ie. Stainless and nickel) should be processed separately to avoid electrolytic action between the different metals. Keep blackened instruments and instruments made from different steels separate to avoid scratches and removal of the black coating.
Care & Handling
The procedures outlined below are recommended to ensure safe handling of biologically contaminated surgical instruments. All instruments must be sterilized before use. NOTE: When reprocessing medical devices always follow local Health & Safety procedures.
Warnings
Follow instructions and warnings as issued by manufacturers of any decontamination, disinfectants and cleaning agents used. Wherever possible, avoid use of mineral acids and harsh, abrasive agents. No part of the process shall exceed 140 degrees C. Some sensitive materials can be damaged by higher alkaline solutions, (pH >10).Note: Single use devices must not be reprocessed and reused.
Limitations on Reprocessing
Repeated processing has minimal effect on the surgical handles, the end of life is normally determined by wear and damage in use.
1. Pre - Cleaning
Wherever possible, do not allow blood, debris or bodily fluids to dry on surgical instruments. For best results and to prolong the life of the medical device reprocess as soon as it is reasonably practical following use. If they cannot be reprocessed immediately, use an enzymatic cleaner to help prevent soil from drying, giving special attention to the blade fitting slots.
2. Cleaning (Cleaning Precautions)
Use an appropriate brush ensuring that it reaches the depth of the slots and threaded holes. Do not use abrasive detergents or cleaning materials. After manually cleaning, pass all devices through an automatic cleaning cycle to achieve disinfection.
a. Automated Cleaning
Use only either CE marked or validated washer- disinfect or machines and low-foaming, non-ionizing cleaning agents and detergents following the manufacturer's instructions for use, warnings, concentrations and recommended cycles. Load instruments carefully so that slots, holes and grooves in the handle can drain. Take care not to overload wash baskets. Ensure that soft, high purity water which is controlled for bacterial endotoxins is used in the final rinse stage.
Note: These instructions have been validated using a washer-disinfectant cycle validated to include:
- one pre-wash stage at a minimum of 320C
- one wash stage at > 600C
- two rinse stages at > 600C and a final disinfectant rinse stage at >900C for a minimum holding time of one minute and a minimum drying stage of thirty minutes.
- The detergent used was an aqueous alkaline wash detergent cleaner with a maximum of pH12 and reverse osmosis water was used for the rinse.
b. Manual Cleaning
Manual cleaning is not advised if an automatic washer-disinfector is available. If this equipment is not available use the following process:
- i. Use a double sink system (wash / rinse) dedicated for instrument cleaning, (not used for hand washing). Ensure that the water temperature does not exceed 35 degrees C.
- ii. In the first sink, keeping the instrument submerged, with an autoclavable brush, apply CE marked cleaning solution to all surfaces until all soil has been removed. Pay particular attention to slots, holes and grooves, always brushing away from the body and avoiding splashing.
- iii. In the second sink rinse, instruments thoroughly with soft, high purity water, which is controlled for bacterial endotoxins so that the water reaches all parts of the instrument, then carefully hand dry or use a drying cabinet.
- iv. After cleaning, visually inspect all slots and grooves for complete removal of soil and fluids. If ANY soil or fluid is still visible, return the instrument for repeat decontamination.
Note: Manual cleaning is NOT a disinfection process: when manual cleaning is used it may not be possible to disinfect the device prior to further handling.
3. Inspection
Visually inspect and check:- All handles that have been cleaned should be thoroughly inspected for any damage or wear within the grooves of the bayonet and any threaded parts. Remove for replacement any worn out or damaged handles.
Note: All instruments to be packed following local protocol in accordance with British Standards.
4. Sterilisation
CE marked or HTM 2010 compliant validated porous steriliser with an air removal stage of 3 negative steam pulses (pressure 1.039 - 0.096 bar a) and five positive steam pulses (0.840 - 2.560 bar a) and a sterilisation temperature of at least 1340C, for a hold time of a minimum of 3 minutes.
Always follow the instructions of the machine manufacturer.
When sterilising multiple instruments in one autoclave cycle, ensure that the manufacturer's stated maximum load is not exceeded.
Ensure instruments are dry prior to sterilisation.
5. Storage
Ensure instruments are dry before storage, and stored in dry, clean conditions at an ambient room temperature.
6. Additional Information
Cleaning and sterilising guidelines are available in HTM 2030, HTM 2010 and BS EN ISO 17665-1 (from all good stationery offices).
NOTE:IT IS THE RESPONSIBILITY OF THE REPROCESSOR TO ENSURE THAT THE REPROCESSING IS ACTUALLY PERFORMED USING EQUIPMENT, MATERIALS AND PERSONNEL IN THE REPROCESSING FACILITY ACHIEVE THE DESIRED RESULT. THIS REQUIRES VALIDATION AND ROUTINE MONITORING OF THE PROCESS. LIKEWISE ANY DEVIATION BY THE REPROCESSOR FROM THE INSTRUCTIONS PROVIDED MUST BE PROPERLY EVALUATED FOR EFFECTIVENESS AND POTENTIAL ADVERSE CONSEQUENCES.